Connect With Us
Blog
Items filtered by date: October 2017
Bunions and How They are Treated
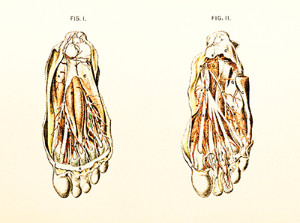
 A bunion is a deformity that occurs on the joint at the base of the big toe. Though the exact cause of bunions is somewhat disputed, wearing tight fitting shoes and genetics tend to play a role in the development and exacerbation of them. Common symptoms that are usually associated with bunions include swelling, soreness, pain, and redness around the joint and bump. Bunions can become worse over time, and poorly-supportive footwear, like high heels, have been associated with worsening them. It is recommended to see a podiatrist when you notice a bunion forming even when it does not cause pain. If you have a bunion that is causing you pain, you should see one right away. A podiatrist will generally offer non-surgical options first if the bunion is not severe. These include bunion pads to relieve pressure off the bunion, pain and anti-inflammatory medication, and suggesting roomier shoes. If the pain continues or worsens and all non-surgical options have failed, surgery may be considered.
A bunion is a deformity that occurs on the joint at the base of the big toe. Though the exact cause of bunions is somewhat disputed, wearing tight fitting shoes and genetics tend to play a role in the development and exacerbation of them. Common symptoms that are usually associated with bunions include swelling, soreness, pain, and redness around the joint and bump. Bunions can become worse over time, and poorly-supportive footwear, like high heels, have been associated with worsening them. It is recommended to see a podiatrist when you notice a bunion forming even when it does not cause pain. If you have a bunion that is causing you pain, you should see one right away. A podiatrist will generally offer non-surgical options first if the bunion is not severe. These include bunion pads to relieve pressure off the bunion, pain and anti-inflammatory medication, and suggesting roomier shoes. If the pain continues or worsens and all non-surgical options have failed, surgery may be considered.
If you are suffering from bunions, contact Dr. Michael T. Hames of Florence Foot Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Florence, Alabama . We offer the newest diagnostic and treatment technologies for all your foot care needs.
New Study Says That Aging Slows Reaction to Falls
 A new study by the University of Waterloo says that the elderly need up to twice as long as young adults to realize they are falling. Seniors are already at an increased risk of falling due to a number of reasons. This study helps show that once they are falling, they don’t process it as quickly as a younger person would. Consequently, there are more times that seniors can’t react fast enough to catch themselves or brace for impact. Falls are a leading cause of hospitalization among the elderly. Studies like this and increased awareness are needed to help prevent future falls among this rapidly growing group of people.
A new study by the University of Waterloo says that the elderly need up to twice as long as young adults to realize they are falling. Seniors are already at an increased risk of falling due to a number of reasons. This study helps show that once they are falling, they don’t process it as quickly as a younger person would. Consequently, there are more times that seniors can’t react fast enough to catch themselves or brace for impact. Falls are a leading cause of hospitalization among the elderly. Studies like this and increased awareness are needed to help prevent future falls among this rapidly growing group of people.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Dr. Michael T. Hames from Florence Foot Center. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Florence, Alabama . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Falls PreventionWhy Do Your Feet Sometimes Get Numb While Working Out?
 Have your feet ever felt numb while you were working out? If so, then you may have experienced paresthesia, a numbness or prickling sensation that many people have temporarily experienced in their life. It is often described as a “pins and needles” sensation that usually goes away once the position of the body changes. Paresthesia is usually caused by a pinched nerve or reduced blood flow to a part of the body. When it comes to working out, the exercises we do can put our body in positions that may reduce blood flow. In other cases, the muscles can swell due to increased blood flow from exercising. Paresthesia is usually a normal condition and often goes away. Not everyone will experience paresthesia or foot swelling, and in most cases it isn’t serious. If, however, your feet have swollen up, feel numb, or you experience pain that doesn’t go away, it is recommended to see a podiatrist.
Have your feet ever felt numb while you were working out? If so, then you may have experienced paresthesia, a numbness or prickling sensation that many people have temporarily experienced in their life. It is often described as a “pins and needles” sensation that usually goes away once the position of the body changes. Paresthesia is usually caused by a pinched nerve or reduced blood flow to a part of the body. When it comes to working out, the exercises we do can put our body in positions that may reduce blood flow. In other cases, the muscles can swell due to increased blood flow from exercising. Paresthesia is usually a normal condition and often goes away. Not everyone will experience paresthesia or foot swelling, and in most cases it isn’t serious. If, however, your feet have swollen up, feel numb, or you experience pain that doesn’t go away, it is recommended to see a podiatrist.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact Dr. Michael T. Hames of Florence Foot Center. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our office located in Florence, Alabama . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Tarsal Tunnel Syndrome?
 Tarsal tunnel syndrome is a condition in which the posterior tibial nerve in the tarsal tunnel becomes pinched or compressed. This causes a number of symptoms including burning and shooting pain, a pins and needles sensation, numbness, and tightness in the foot. There are several reasons why the nerve could become compressed, which include bony prominences, bone spurs, abnormal heel position, and the swelling of tendons in the tarsal tunnel. Due to the nature of tarsal tunnel syndrome, diagnosis may be difficult because it can seem to mimic the symptoms of other conditions; heel pain and arch pain are some examples. It is best to see a podiatrist if you are experiencing any of those symptoms. Podiatrists can offer a number of treatments, such as orthotics, taping or bracing, rest, icing, anti-inflammatory medication, or even surgery if other treatments do not improve your condition.
Tarsal tunnel syndrome is a condition in which the posterior tibial nerve in the tarsal tunnel becomes pinched or compressed. This causes a number of symptoms including burning and shooting pain, a pins and needles sensation, numbness, and tightness in the foot. There are several reasons why the nerve could become compressed, which include bony prominences, bone spurs, abnormal heel position, and the swelling of tendons in the tarsal tunnel. Due to the nature of tarsal tunnel syndrome, diagnosis may be difficult because it can seem to mimic the symptoms of other conditions; heel pain and arch pain are some examples. It is best to see a podiatrist if you are experiencing any of those symptoms. Podiatrists can offer a number of treatments, such as orthotics, taping or bracing, rest, icing, anti-inflammatory medication, or even surgery if other treatments do not improve your condition.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Dr. Michael T. Hames of Florence Foot Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Florence, Alabama . We offer the newest diagnostic and treatment technologies for all your foot need.
Read more about Tarsal Tunnel SyndromeBlog Archives
- December 2025
- November 2025
- October 2025
- September 2025
- August 2025
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
